Why are dental implants needed?
Once a tooth is lost, its surrounding supporting bone gradually deteriorates in quality and quantity, leading to loss of bone volume. Your dentist may recommend different treatment options and procedures to replace your missing tooth and restore your compromised appearance, speech and chewing comfort.
A dental implant is an alloplastic artificial screw-type medical device which is placed into the jawbone to support an artificial crown. Like a tooth root, a single implant is firmly attached or integrated into the jawbone. Implants are either made from commercially pure titanium or Zirconium, called Zirconia ceramic implants.
Although dental implants may require more time, expenses, and technical expertise, they offer a few advantages in terms of more long-term functional stability and less invasiveness to the adjacent tissues and teeth.
An implant could be placed “immediately” or in a “delayed” or “late phase” after the tooth is extracted to preserve the jawbone. In cases of residual acute infection, a delayed surgical approach is preferred to minimise the infection risk.
Titanium and zirconium are very inert materials that could be firmly attached or integrated with the bone to provide support for a crown like that of a tooth root. If an implant is placed immediately or shortly after a tooth is extracted, the jawbone will be more preserved against future bone resorption. Unless a considerable amount of bone resorption has taken place, placement of an implant is usually possible when additional bone grafting techniques are undertaken.


What procedures and timelines are involved in the placement of the implant?
Phase 1: Case assessment
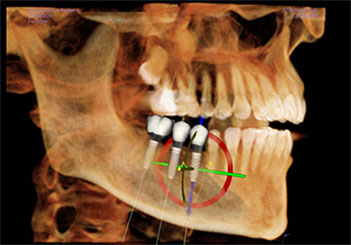
Following an implant consultation, further diagnostic clinical and radiographic investigation (X-rays), e.g. CBCT-scan, is required to ascertain the availability and to determine implant location and 3-dimensional implant positioning. Sometimes, further site information about the jawbone’s quality and quantity and the choice of implant placement protocol will be obtained at the time of surgery.
If the clinical examination reveals that the bone around the infected tooth root is severely resorbed, the resorbed bone requires bone augmentation. The options for the treatment of the missing tooth would be a delayed implant placement after atraumatic extraction and a more extended healing period. The advantage is an improved implant primary stability following partial bone healing, increased post-healing gum availability, and complete resolution of remnant infection.
When there is sufficient bone height but not bone width, implant placement may require lateral bone augmentation before implant placement. Implant placement will be undertaken six months after bone augmentation, and the implant crown restoration will be conducted 3 months after implant placement.
If there is sufficient bone height and width at the site of implant placement, bone augmentation is not required, and the Implant-crown restoration could be undertaken two months after implant placement.
When there is sufficient bone width but not bone height for implant placement under the sinus floor, the implant placement does require sinus floor bone augmentation, and the implant crown restoration will be undertaken six months after implant placement.
Phase 2: Implant placement
Once the bone topography is re-evaluated during the surgery, the dental implant is placed under sterile conditions and local anaesthetic.
As a result of tooth extraction, dental infection, trauma, or post-operative bone resorption, it would be necessary to reconstruct or augment the bony ridge defect around the missing teeth before or simultaneous to implant placement. Therefore, to ensure that there is sufficient bone around the implant, the alveolar ridge may need to be restored to ensure a long-lasting and stable tooth replacement utilising dental implants.
For minor bone deficiencies, guided bone regeneration may be implemented. This may involve the use of a membrane which acts as a biological barrier to promote bone regeneration and mineralisation around the defective alveolar ridge. The barrier prevents other cells from growing into the defect, which enables merely the bone cells’ ingrowth.
Guided bone regeneration or ‘augmentation’ procedure is performed using a variety of techniques and materials, including human/animal-derived and synthetic products. The patient’s bone or a mixture of all these may be used based on the amount of bone required.
Phase 3 Healing period
The patient will be reviewed weekly for follow-up on the tissue healing and possible suture removal. After 6-10 days, once the soft tissues have healed sufficiently, the stitches may be removed. During this period, wearing dentures or temporary restorations may be impossible. After this stage, the implants will usually be left undisturbed for up to six months to attach to the jawbone. To modify the soft tissue healing, immediate provisional restoration may be placed to optimise the definitive crown’s bite, colour, position, projection, and shape.
Phase 4 Restorative phase
After 2 to 6 months, a second localised surgical procedure may be necessary to expose the implant(s) and check for implant integration. If an implant has failed to take, it can be removed, as it will not be attached to the bone. Once the implant(s) have been uncovered and firm, a post or abutment will be connected, which will support a provisional crown.
During the final restorative treatment phase, an analogue or digital impression will be provided to design and fabricate the final crown. Then, the implant will be restored, and the patient will start chewing on the new tooth.
Phase 5 Function & maintenance
During the maintenance phase of the implant treatment, regular hygiene visits and check-ups are planned quarterly or biannually to prevent and intervene with any possible inadvertent risk for biological or mechanical complications around your functional dental implants.
Types of implant-supported prostheses:
Implant-supported single crown
When a single tooth is missing, the alternative treatments could be either the fabrication of a conventional bridge or a partial denture.
The advantages of the provision of an implant-supported single crown are the following: the implant is fixed and does not move; the Implant does not get decayed; the implant does not require cutting the adjacent teeth; it is easier to clean and implant crown than a bridge; implant-crown has well -documented success and longevity; implant prevents further bone loss.
The disadvantages of the provision of an implant-supported single crown are the following: implant treatment requires longer treatment time, requires surgery, and involves higher costs.
Implant-supported bridge
An implant-supported bridge requires more than one implant unit, depending on how many missing teeth are replaced. It has advantages and disadvantages similar to the single implant crown, except for further treatment time, cost, and planning requirements.
Implant-supported All-on-4 or All-on-6 cross-arch bridge
The concept of All-on-4 or All-on-6 implants for any implant system is based on a fixed rehabilitation of missing teeth utilising immediate placement and loading of four or six dental implants with a provisional fixed bridge. This requires a careful and comprehensive treatment planning procedure encompassing CBCT radiography, sophisticated surgical procedures, and laboratory stages, converting the provisional bridge to the final full-arch prosthesis.
Based on the recent scientific literature reviews, it has been concluded that only two appropriately placed posterior respective anterior implants are deemed to adequately support a fixed prosthesis and avoid the need for undertaking any major bone grafting procedures.
Implant-supported removable prostheses and over-dentures
Over-denture is a favourable simplified prosthetic treatment modality for elderly patients. There are fewer implants involving limited traumatic surgical invasion, and less clinical chairside time- and financial- resources are required.
There are instances where, due to the extensive atrophied residual alveolar bone, the provision of the conventional implant-supported fixed prosthesis (ISFP) is not clinically feasible. Under these circumstances, only a few implants could be placed in the jaws’ front region, rendering implant-retained overdentures (ISOD) a viable and predictable treatment modality. Furthermore, this alternative also facilitates the replacement of lost hard and soft tissue, especially in patients with congenital/acquired defects, to improve aesthetics and phonetics and avoid food entrapment.
Are all the implants the same?
The long-term success rate for each dental implant placed in your jawbone is determined by certain factors that directly affect the time and cost involved in providing implant-supported prostheses.
The cost of the implants and implant-supported prostheses is determined by the factors below:
- The surgeon’s level of education and experience and specialisation in surgical aspects of implantology.
- The prosthodontist’s level of expertise and specialisation in restorative aspects of dental implantology.
- The implant technical fabrication procedures and chemo-physical surface treatment.
- The type of post/abutment connection and quality.
- The clinic’s quality control protocols.
- The technician’s expertise and prosthesis quality in design and manufacturing processing.
Dr Nico Kamosi and his team at London Specialist Dentists utilise implant systems from the world-leading Swiss and Swedish companies with the lowest rate of biological and biomechanical complications or failures. We have more than two decades of expertise in both surgical and restorative aspects of dental implantology.

When are bone regeneration or augmentation procedures performed?
As a result of tooth extraction, dental infection, trauma and post-operative bone resorption, it would be necessary to reconstruct or augment the soft tissue and bony ridge defects simultaneously or before implant placement to ensure that there is sufficient bone around the implant. In addition, the alveolar ridge may need to be restored to ensure a long-lasting and stable tooth replacement utilising dental implants.
In the absence of bone augmentation, bone defects may develop around the neck of the implant, which would result in aesthetic and biological complications, especially in the aesthetic zone. Although bone grafting procedures are often very successful, some biological complications, such as graft infection or resorption, may interfere with successful integration and consolidation.
Both the function and the aesthetics of the implant-supported teeth can be severely compromised when the supporting bone and gum are deficient.
For minor bone deficiencies, guided bone regeneration or ‘augmentation’ procedure may be implemented using a variety of techniques and materials, including human or animal-derived and synthetic products. This may involve the use of a membrane which acts as a biological barrier to promote bone regeneration around the defective alveolar ridge. The barrier membrane prevents other cells from growing into the defect to promote selective ingrowth of bone cells.
Read more about bone regeneration or augmentation materials and techniques.
When is the maxillary sinus augmentation procedure performed?
Sinus spaces are cavities in the upper jaw (Maxilla) on each side of the nose and above your upper back teeth. When there is too little bone at the back of the upper jaw, sinus augmentation is performed to increase the amount of supporting bone around the implants. Sinus grafting is a technique-sensitive procedure which requires surgical and prosthodontic skills. However, despite complications such as tearing of the sinus membrane, infection of the graft, or loss of the implants, any long-term sinus complication rarely occurs. A review of sinus biopsy after the sinus grafting indicates that bone can form from the sinus floor with every graft material when the sinus lining and the wound environment are maintained intact. Autogenous bone is highly osteoinductive and promotes sinus augmentation in synergy with sinus floor inherent bone migration.
When does a dental implant not integrate?
As with any surgical treatment, research shows that only about 2-5% of implants may fail. Should an implant fail to integrate, it is often possible to replace it with a second implant simultaneously or some weeks after the first implant is removed. It has been shown that systemic factors, including alcohol consumption and local factors like tobacco, may compromise tissue healing, implant integration and implant success rate.
The soft tissues around the implant are relatively resistant to infection. However, in the absence of regular self-performed plaque control and hygiene appointments, the gum around the implant may bleed, and gradually, the inflammation may progress into advanced bone loss around your implants. This could result in their eventual failure.
Is it necessary to attend maintenance appointments after the implant placement?
Upon completion of the implant therapy, you should attend the same clinic for regular maintenance appointments to assess the tissues around your implant and the crown. The frequency of hygienist visits will depend on your standard of oral hygiene. Long-term maintenance of the implant and crown will be required, as for any other standard crown.
Minor maintenance may include removing the crown to check the implant abutment and replacement of retention screws when required. Major maintenance may involve the replacement of the crown due to wear and tear. These maintenance requirements will incur additional costs above the initial fees.
FAQ – What do patients usually ask about dental implant?
In most of the cases, we can provide you with a provisional tooth or teeth which would replace the missing tooth. When the implant provides adequate primary stability, we could even fabricate a provisional crown immediately connected and supported on your implant. The implant integration period could take a period of 6 to 20 weeks dependent on its surrounding supporting bone at the time of surgery.
As for any localised dental surgery: minor bleeding, bruising, swelling, discomfort may occur dependent on the extent of the implant surgery e.g., bone grafting. Both bruising or swelling will usually be alleviated after 48 hours after the procedure. The local discomfort is well controlled when using pain killers such as Ibuprofen. In extremely rare cases an antibiotic may be prescribed. When premium-branded implant is used, the dental implant the failure rate is very low (1%). Obviously, patients who smoke or suffer from uncontrolled diabetes or gum-disease are at a higher failure risk. An individualised implant protocol is made to minimise such risk.
In principle, anyone over the age of 18 years old is suitable for dental implants. Albeit, some medical conditions such as bleeding disorders would make ant surgery very difficult. Other precautions are side effects from certain drugs e.g. bisphosphonates, immunosuppressant which can be discussed with your doctor when indicated. After a full dental and medical assessment, the appropriateness of implant surgery will be discussed between your dentist and your physician after your initial consultation.
As for natural teeth, regular maintenance care by a hygienist and dentist is required for your dental implants. There is a body of scientific evidence showing that most of the premium implant system have a survival rate of 80 to 90% during 10-15 years of service.
Identified risk indicators for biological complication may include: poor oral hygiene, history of periodontitis, uncontrolled diabetes and heavy smoking, coupled with compromised host tissues or immune response. Therefore, the above-mentioned risk factors should be monitored, and kept under optimal control.
The standard of oral hygiene should be reinforced and general health status of the periodontal tissues around the remaining teeth should be monitored during the maintenance phase.
Shallow residual pockets should be monitored regularly and treated if signs of disease activity are noticed. If you are smoker this habit adversely affects your periodontal and peri-implant health & long-term prognosis for the treatment outcome.
The Guarantee for your dental implant is issued for a year after the insertion. This does not cover failure due to poor oral hygiene, history of periodontitis, uncontrolled diabetes and heavy smoking, or compromised host tissues or immune response, misuse or accidents.
Our clinic undertakes to warrant implant-supported crowns, bridges and prostheses against mechanical failure for three years. The guarantee is subject to your compliance with the highest standard of oral hygiene and regular attendance for maintenance and reviews recommended every 4 months. You should attend the dental hygienist/ dentist regularly every 6 months for professional hygiene and maintenance of the restorations provided. You should undertake any remedial treatment regarded as necessary to maintain you dental and implant health. Therefore, we strongly recommend all of our patients who have received implant treatment to undertake radiographic and other investigations on an annual basis to review the stability of the implant.
Periodontists are further qualified and have comprehensive training in the diagnosis and treatment of disease around your teeth and dental implants. They are highly-skilled surgeons and have advanced in Restorative dentistry which encompasses expertise in planning, placement and restoration of your dental implants.
Dental Implant Case Studies
See our dental implant before and after photos from our happy patients.

Before and After Treatment
Aesthetically disturbing smile line, uncomfortable partial prosthesis.

Before and After Treatment
Missing teeth, periodontally deteriorated teeth, reversed occlusal relationship and collapsed bite.


